Living with Parkinson’s: A Solid Guide for Seniors!

Last Updated on June 30, 2025 by George
Navigating life with Parkinson’s disease presents unique challenges, but with the right knowledge and support, seniors can maintain independence and find joy in each day. This comprehensive guide offers practical insights for those recently diagnosed and their caregivers.
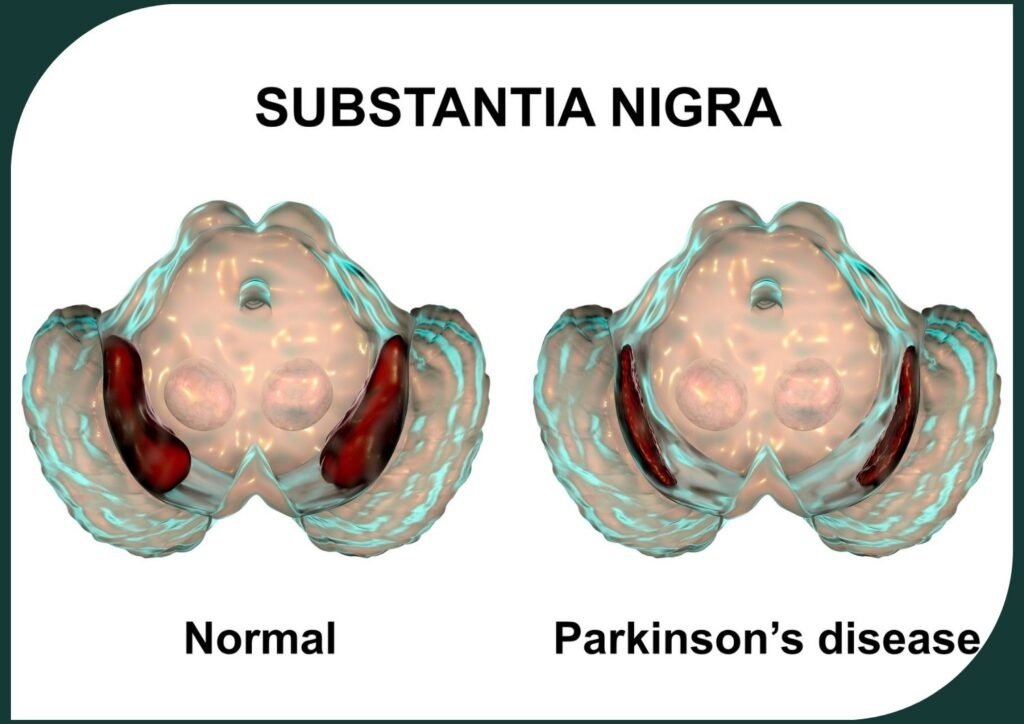
Parkinson’s disease occurs when dopamine-producing cells in the brain’s substantia nigra begin to deteriorate. According to recent studies from the Michael J. Fox Foundation (2023), approximately 1 million Americans currently live with Parkinson’s, with 60,000 new diagnoses each year. While there’s currently no cure, remarkable advances in treatment options have dramatically improved quality of life outcomes.
Understanding Parkinson’s begins with recognizing its early signs—subtle tremors, changes in handwriting, reduced arm swing while walking, and voice softening. These initial symptoms often appear gradually, sometimes years before a formal diagnosis. Recent research published in the Journal of Neurology (2024) suggests that non-motor symptoms like sleep disturbances and loss of smell may actually precede motor symptoms by up to a decade.
This guide explores:
- The science behind Parkinson’s and its progression
- Effective strategies for managing common symptoms
- Latest treatment approaches, including medication innovations and therapy advances
- Home adaptation tips for maintaining independence
- Nutritional guidance specifically tailored for Parkinson’s
- Self-care practices for emotional well-being
- Essential support resources for patients and caregivers
Whether you’re newly diagnosed or supporting a loved one, you’ll discover practical tools to transform challenges into opportunities for adaptation and growth. Are you ready to explore how to embrace life with Parkinson’s with confidence and resilience?
Understanding the Science Behind Parkinson’s
Parkinson’s disease is a neurodegenerative disorder that primarily affects the motor system. According to the latest research from the American Parkinson Disease Association (2023), this condition develops when a significant number of dopamine-producing neurons in the substantia nigra region of the brain begin to deteriorate.
The substantia nigra plays a critical role in movement control and coordination. It produces dopamine, which transmits signals between nerve cells to help regulate and smooth our movements. When dopamine levels decline by about 60-80%, the characteristic motor symptoms of Parkinson’s begin to appear.
Recent studies published in Nature Neuroscience (2024) have expanded our understanding of Parkinson’s beyond dopamine depletion. Researchers now recognize that Parkinson’s also involves abnormal accumulation of a protein called alpha-synuclein, which forms clumps called Lewy bodies within neurons, potentially contributing to cell dysfunction and death.
Scientists at the Mayo Clinic have recently identified that this process may actually begin in the gut and olfactory bulb years before reaching the brain’s movement centers, explaining why symptoms like constipation and reduced sense of smell often precede motor symptoms.
Prefer to listen rather than read?
Early Signs and Symptoms: Catching Parkinson’s Early
Parkinson’s typically begins subtly, with symptoms that might be mistaken for normal aging. According to neurologist Dr. Rachel Dolhun of the Michael J. Fox Foundation: “Recognizing these early signs can lead to earlier intervention and better long-term outcomes.” Common early symptoms include:
Resting Tremors
One of the most recognizable symptoms is a slight tremor or shaking, typically beginning in one hand, finger, or thumb while at rest. You might notice this as a “pill-rolling” motion between thumb and forefinger. Unlike essential tremor, Parkinson’s tremors generally subside during purposeful movements.
These tremors often begin on one side of the body before potentially progressing to both sides. Unlike action tremors, they’re most noticeable when the limb is relaxed and supported.
Bradykinesia (Slowness of Movement)
Bradykinesia describes the frustrating slowness in initiating and carrying out movements. Simple tasks like buttoning a shirt or cutting food become time-consuming challenges. Research from the University of California (2023) found that this symptom significantly impacts quality of life, often before more visible symptoms appear.
Dr. James Beck, Chief Scientific Officer at the Parkinson’s Foundation, explains: “Bradykinesia isn’t just physical slowness—it’s the brain’s difficulty in translating intention into action. This disconnect explains why patients know what they want to do but struggle to execute the movement.”
Muscle Rigidity
Muscle stiffness can affect various body parts, creating resistance during movement. This rigidity, described by patients as feeling like moving through molasses, contributes to a decreased range of motion and sometimes pain. Physical therapists specializing in Parkinson’s recommend consistent stretching exercises to counteract this symptom.

Postural Instability
As Parkinson’s progresses, maintaining balance becomes increasingly challenging. This manifests as a tendency to lean or sway when standing, potentially increasing fall risk. According to a 2023 study in the Journal of Neurology, implementing balance training early can delay serious mobility issues by up to three years.
Non-Motor Symptoms
Beyond movement difficulties, Parkinson’s can cause:
- Sleep disturbances, particularly REM sleep behavior disorder
- Reduced sense of smell
- Constipation
- Changes in handwriting (typically becoming smaller)
- Voice changes (becoming softer or more monotone)
- Facial masking (reduced facial expressions)
Dr. Lisa Shulman, Professor of Neurology at the University of Maryland, notes: “Many patients report these non-motor symptoms were present for years before their tremor or movement issues led to diagnosis.”
Advanced Symptoms: What to Expect as Parkinson’s Progresses
As Parkinson’s advances, symptoms may expand and intensify. Being aware of these changes helps patients and caregivers prepare and implement appropriate management strategies.
Freezing of Gait
This sudden, temporary inability to move forward despite the intention to walk can be particularly distressing. It often occurs when approaching doorways, making turns, or navigating crowded spaces.
Researchers at the University of Pennsylvania have identified that visual cues—like lines on the floor—can help overcome freezing episodes. Their 2023 study demonstrated a 45% reduction in freezing incidents when patients used rhythmic auditory or visual cues.
Speech and Swallowing Difficulties
Parkinson’s can affect the muscles involved in speech and swallowing, potentially leading to:
- Softer, monotone speech (hypophonia)
- Slurred or mumbled words
- Rapid speech that’s difficult to understand
- Difficulty swallowing (dysphagia)
These changes can significantly impact communication and nutrition. Speech-language pathologists play a crucial role in maintaining these functions through specialized therapy programs like LSVT LOUD, which has shown significant benefits in preserving communication abilities.
Aspiration pneumonia occurs when food or liquid accidentally enters the airway, leading to lung infections. This emphasizes the importance of seeking professional guidance and support for individuals affected by Parkinson’s. Early intervention and expert care are key to maintaining a high quality of life.
Cognitive Changes
Many people with Parkinson’s experience cognitive challenges ranging from mild executive function difficulties to more significant cognitive decline. Recent research from Johns Hopkins University (2023) found that regular cognitive stimulation through activities like puzzle-solving and language learning may help maintain cognitive function.
These cognitive aspects of Parkinson’s can be as impactful as the physical symptoms, affecting:
- Decision-making abilities
- Multi-tasking capabilities
- Short-term memory
- Information processing speed
Mood and Emotional Changes
Depression, anxiety, and apathy frequently accompany Parkinson’s, stemming from both neurochemical changes and adjustment to living with a chronic condition. According to the Parkinson’s Foundation, approximately 50% of patients experience depression, and up to 40% deal with anxiety—rates significantly higher than in the general senior population.
Dr. Indu Subramanian, Director of the Parkinson’s Disease Research, Education, and Clinical Center at UCLA, emphasizes: “These aren’t just reactions to having Parkinson’s—they’re actually part of the disease process itself as Parkinson’s affects brain regions that regulate mood.”
Living Well with Parkinson’s: Daily Management Strategies
Living with Parkinson’s extends beyond managing symptoms—it’s about embracing a full life with adaptation and resilience. By implementing thoughtful strategies, seniors with Parkinson’s can maintain independence and joy.
Establishing a Consistent Daily Routine
One of the most effective approaches to managing Parkinson’s is creating a structured daily schedule. The predictability provides stability while maximizing periods of good mobility. Neurologists recommend organizing activities around medication timing, when symptoms are typically best controlled.
A beneficial daily structure might include:
Morning Ritual
Begin your day with gentle stretching exercises that target Parkinson’s-specific issues like rigidity and reduced range of motion. The American Parkinson Disease Association recommends starting with these movements while still in bed:
- Ankle rotations (10 each direction)
- Knee to chest holds (hold for 10 seconds each side)
- Gentle trunk rotations
Follow with a nutritious, high-fiber breakfast to address common digestive challenges.
Medication Management
If you’re taking medication for Parkinson’s (such as levodopa/carbidopa), timing becomes crucial for symptom control. Using pill organizers with alarms helps maintain consistent dosing. The Fox Foundation’s 2023 patient survey found that medication timing apps significantly improved adherence and symptom management.
Dr. Daniel Truong, neurologist and Parkinson’s specialist, advises: “Take medications consistently—not just at the same times each day, but also with respect to meals, as protein can affect levodopa absorption.”

Activity Planning
Plan your most demanding activities during your “on” periods when medication is working optimally. Reserve lighter activities for potential “off” periods. Breaking tasks into smaller steps prevents fatigue and frustration.
Home Adaptations for Safety and Independence
Simple environmental modifications can dramatically improve safety and facilitate independence:
- Install grab bars in bathrooms and near steps
- Remove trip hazards like loose rugs and clutter
- Improve lighting, especially in hallways and stairwells
- Consider chair risers for easier standing
- Replace round doorknobs with lever handles
- Use adaptive utensils with weighted, larger-grip handles
- Add motion-sensor lights for nighttime navigation
Occupational therapist Jennifer Garland recommends: “Don’t wait for problems to implement changes. Proactive adaptation prevents falls and preserves independence.”
Exercise: The Non-Negotiable Treatment
Exercise is now considered essential treatment for Parkinson’s, not just a supplement to medication. Research published in Neurology (2023) demonstrated that patients engaging in regular exercise showed significantly slower disease progression than sedentary counterparts.
Effective exercise programs for Parkinson’s include:
- PWR! (Parkinson Wellness Recovery) – Focuses on large, functional movements that counteract the shrinking movement patterns of Parkinson’s
- LSVT BIG – Emphasizes exaggerated movements to overcome bradykinesia
- Tai Chi – Improves balance and prevents falls (a 2023 study showed a 60% reduction in falls among practitioners)
- Dance therapy – Particularly tango and other rhythmic dances that improve gait and balance
- Cycling – Research indicates cycling may temporarily reduce tremors and rigidity
- Aquatic exercise – Provides resistance while supporting balance
Dr. Jay Alberts, researcher at the Cleveland Clinic, notes: “We’ve found that forced exercise—maintaining a consistent, somewhat challenging pace—appears particularly beneficial for Parkinson’s symptoms.”
Aim for at least 150 minutes of moderate exercise weekly, divided into manageable sessions.
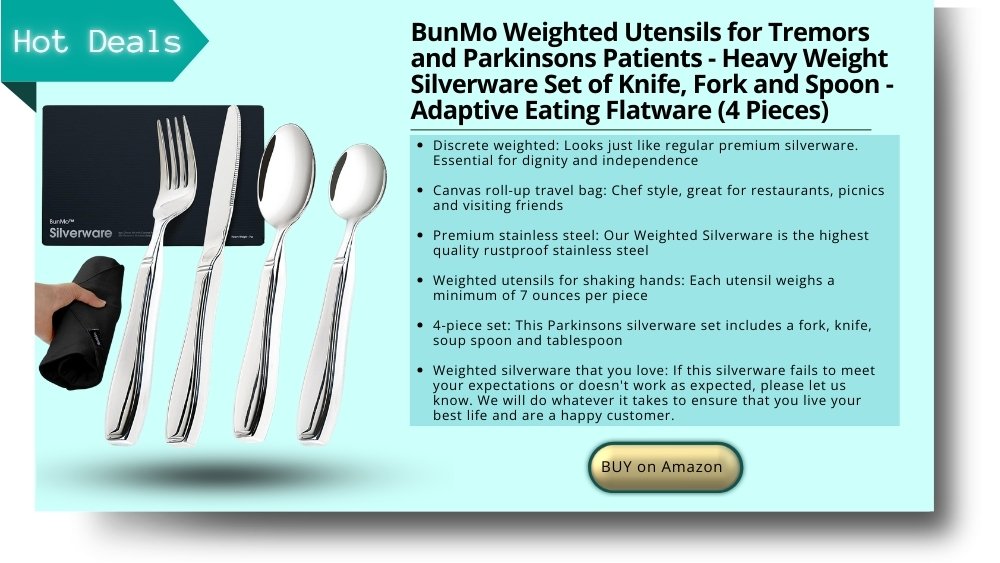
Utilize Assistive Devices
Incorporating assistive devices into your daily life can make a significant difference. These tools are designed to aid you in various tasks, promoting independence and reducing physical strain. Here are some recommendations:
- Walking Aids
- Consider walking poles rather than traditional canes—they promote a more upright posture and natural gait pattern while providing stability. The Parkinson’s Foundation recommends U-Step walkers specifically designed with features that help prevent freezing.
- Tremor-Reducing Equipment
- Weighted utensils and cups can significantly reduce eating difficulties. The latest adaptive technologies include electronic spoons that counteract tremors, allowing greater mealtime independence.
- Voice Amplification
- Wearable voice amplifiers address hypophonia (soft speech), ensuring better communication without strain. Speech pathologists can recommend appropriate devices based on individual needs.
- Smart Home Technology
- Voice-activated systems can control lighting, temperature, and appliances, reducing the need for fine motor control. Many seniors find these systems provide both practical assistance and increased safety.
Regular Healthcare Collaboration
Effective Parkinson’s management requires a multidisciplinary approach. The American Academy of Neurology recommends regular consultations with:
- Neurologist (ideally a movement disorder specialist)
- Physical therapist with Parkinson’s expertise
- Occupational therapist for daily living adaptations
- Speech-language pathologist for communication and swallowing
- Nutritionist for Parkinson’s-specific dietary guidance
- Mental health professional for emotional wellbeing
Dr. Michael Okun, Medical Director of the Parkinson’s Foundation, emphasizes: “The difference between seeing a general neurologist versus a movement disorder specialist can be significant in terms of quality of care and access to the latest treatments.”
Your journey with Parkinson’s is unique, and it’s crucial to have a reliable healthcare team by your side. Regular consultations with healthcare professionals, including neurologists, physical therapists, and occupational therapists, can help you manage your condition effectively.

Supporting Loved Ones with Parkinson’s: A Guide for Caregivers
Caring for someone with Parkinson’s requires both practical skills and emotional resilience. As a caregiver, your support creates the foundation for your loved one’s quality of life.
Education and Understanding
Learning about Parkinson’s is your first essential step. The more you understand about the disease’s mechanisms and progression, the better you can anticipate and address changing needs. Dr. Rachel Dolhun recommends: “Attend medical appointments when possible. Ask questions. Take notes. Become an informed advocate.”
Online courses specifically for Parkinson’s caregivers are available through organizations like the Parkinson’s Foundation and the Michael J. Fox Foundation.
Patience and Empathy
Parkinson’s symptoms fluctuate unpredictably, which can be frustrating for both the patient and caregiver. Understanding that slowness, freezing, or difficulty communicating are disease symptoms—not choices—helps maintain a positive relationship.
Remember that your loved one may be struggling with invisible symptoms like pain, fatigue, or anxiety alongside visible motor issues. Dr. Soania Mathur, a physician living with Parkinson’s, advises: “Ask about these hidden challenges. Sometimes just acknowledging them provides significant relief.”
Practical Support Strategies
Effective caregiving balances assistance with independence:
- Allow extra time for tasks rather than taking over
- Suggest rest breaks before frustration builds
- Use gentle prompting rather than criticism
- For freezing episodes, offer visual cues like asking the person to step over an imaginary line
- During “off” periods, prioritize comfort and safety
- Maintain dignity during personal care by offering choices and privacy
- Learn proper transfer techniques to prevent injury to both yourself and your loved one
Self-Care Is Essential
Caregiver burnout presents a real risk in progressive conditions like Parkinson’s. A 2023 study in The Gerontologist found that caregivers who practiced consistent self-care provided better support and experienced less depression.
Vital self-care practices include:
- Joining a caregiver support group (in-person or online)
- Accepting help from others and using respite care
- Maintaining your own healthcare appointments
- Pursuing activities that bring you joy and renewal
- Setting realistic expectations and boundaries
- Connecting with supportive friends and family
Gerontologist Dr. Julie Carter emphasizes: “Caregiver self-care isn’t selfish—it’s necessary for sustainable care. Your loved one benefits when you’re physically and emotionally well.”

Treatment Approaches: Current Options and Emerging Horizons
While there’s currently no cure for Parkinson’s, treatment options continue to expand, offering better symptom control and quality of life.
Medication Therapies
Medication remains the cornerstone of Parkinson’s treatment. Recent advances have improved delivery methods and reduced side effects:
Levodopa-Based Treatments
Levodopa (usually combined with carbidopa) remains the most effective medication for motor symptoms. Recent developments include:
- Extended-release formulations that provide more consistent symptom control
- Inhaled levodopa (Inbrija) for rapid relief during “off” periods
- Intestinal gel infusion (Duopa) for advanced cases with severe fluctuations
Neurologist Dr. Melissa Armstrong notes: “The goal isn’t just to provide levodopa, but to maintain steady dopamine levels throughout the day, minimizing fluctuations.”
Dopamine Agonists
These medications stimulate dopamine receptors directly and include pramipexole (Mirapex), ropinirole (Requip), and rotigotine (Neupro patch). They’re often used in early Parkinson’s or in combination with levodopa.
MAO-B and COMT Inhibitors
These medications slow the breakdown of dopamine, prolonging levodopa’s effectiveness. Recent research in the Journal of Parkinson’s Disease (2023) showed that combining these with appropriate levodopa timing reduced “off” time by up to 1.5 hours daily.
Medical Cannabis
Research on medical cannabis for Parkinson’s has expanded significantly. A 2023 review in Movement Disorders indicated potential benefits for non-motor symptoms like sleep disturbances, pain, and anxiety, though effects on motor symptoms appear more variable.
Dr. James Beck cautions: “While some patients report benefits, cannabis research for Parkinson’s is still developing. Patients should discuss this option with their movement disorder specialist rather than self-medicating.”
Physical and Occupational Therapy
Specialized therapy programs have demonstrated remarkable benefits:
- LSVT BIG therapy uses exaggerated movements to overcome bradykinesia, with benefits lasting up to two years after the initial four-week program
- PWR! (Parkinson Wellness Recovery) integrates functional movements into daily activities
- Dutch ParkinsonNet approach provides coordinated, specialized care through trained therapists
A 2023 study in Physical Therapy journal found that Parkinson’s-specific therapy protocols improved mobility measures by 32% compared to general physical therapy.
Surgical Interventions
For some patients, surgical options offer significant symptom relief when medications become less effective:
Deep Brain Stimulation (DBS)
This procedure involves implanting electrodes in specific brain regions to deliver controlled electrical stimulation. Recent advances include:
- Directional leads that allow more precise stimulation and fewer side effects
- Adaptive systems that respond to changing symptoms in real-time
- MRI-compatible devices for easier follow-up monitoring
Neurosurgeon Dr. Helen Bronte-Stewart explains: “Modern DBS systems give us unprecedented control. We can now target symptoms with remarkable precision while minimizing side effects.”
Research from 2023 shows that earlier intervention with DBS—before severe complications develop—may provide better long-term outcomes than the traditional approach of waiting until advanced disease.
Focused Ultrasound
This non-invasive procedure uses sound waves to precisely target and treat small areas of the brain. In 2023, the FDA expanded approval for focused ultrasound to include more Parkinson’s symptoms, providing an option for patients who cannot or prefer not to undergo traditional surgery.
Complementary Approaches
While not replacements for medical treatment, several complementary approaches show promise:
- Mindfulness meditation – A 2023 study demonstrated improvements in anxiety, depression, and sleep quality
- Acupuncture – May provide modest benefits for pain and some non-motor symptoms
- Music therapy – Particularly effective for gait training and mood improvement
- Massage therapy – Can temporarily reduce rigidity and improve comfort
Dr. Benzi Kluger of the University of Rochester advises: “These approaches work best as complements to, not replacements for, conventional care. The ideal approach integrates evidence-based conventional and complementary methods.”
Nutrition and Diet: Fueling Your Body with Parkinson’s
Proper nutrition plays a vital role in managing Parkinson’s symptoms and medication effectiveness. Recent research has clarified specific dietary approaches that may benefit those with Parkinson’s.
Mediterranean Diet Benefits
A 2023 study in the Journal of Neurology found that adherence to a Mediterranean diet was associated with slower Parkinson’s progression and better quality of life. This approach emphasizes:
- Abundant vegetables, fruits, and whole grains
- Olive oil as the primary fat source
- Regular consumption of fatty fish rich in omega-3s
- Limited red meat consumption
- Moderate intake of dairy, eggs, and wine
Nutritionist and Parkinson’s specialist Dr. Laurie Mischley notes: “The anti-inflammatory properties of the Mediterranean diet appear particularly beneficial for neurodegenerative conditions like Parkinson’s.”
Protein Timing and Medication Effectiveness
For many taking levodopa, protein intake can affect medication absorption and effectiveness. Registered dietitian Katherine Grandinetti explains: “Protein and levodopa compete for absorption in the small intestine. Strategic timing can improve symptom management.”
Options for managing this interaction include:
- Taking levodopa 30-60 minutes before meals
- Adopting a “protein redistribution diet” with lower protein during the day and higher protein at dinner
- Consulting with a dietitian to create an individualized plan that maintains adequate nutrition while optimizing medication effectiveness
Managing Common Nutritional Challenges
Parkinson’s can present several nutrition-related difficulties:
Constipation
Nearly 60% of people with Parkinson’s experience constipation due to slowed digestive motility and medication side effects. Nutritional strategies include:
- Gradually increasing fiber intake to 25-35 grams daily
- Ensuring adequate hydration (aim for 64 ounces of fluid daily)
- Including probiotic foods like yogurt and kefir
- Adding ground flaxseed to foods (start with 1 teaspoon daily and increase slowly)
- Establishing a regular eating schedule to promote digestive regularity
Swallowing Difficulties
As Parkinson’s progresses, dysphagia (difficulty swallowing) may develop. Signs include coughing during meals, unexplained weight loss, or food “sticking” in the throat. Working with a speech-language pathologist is essential for specific recommendations, which might include:
- Modifying food textures (softer foods may be easier to manage)
- Proper positioning during meals (sitting upright with chin slightly tucked)
- Swallowing techniques like the “effortful swallow” or “supraglottic swallow”
- Thickened liquids if thin liquids cause coughing

Weight Management
Some with Parkinson’s experience unintended weight loss due to increased energy expenditure from tremors, decreased appetite, or swallowing difficulties. Others may gain weight due to reduced mobility. Tailored nutritional guidance can address these opposing challenges.
Specific Nutrients of Interest
Research has identified several nutrients of particular interest for Parkinson’s:
Antioxidants
People with Parkinson’s typically show higher levels of oxidative stress. Colorful fruits and vegetables rich in antioxidants may help counteract this effect. Particularly beneficial options include:
- Berries (especially blueberries and blackberries)
- Dark leafy greens
- Bright orange vegetables like sweet potatoes and carrots
- Green tea
Omega-3 Fatty Acids
Found primarily in fatty fish, flaxseed, and walnuts, omega-3s have anti-inflammatory properties that may benefit brain health. A 2023 study in Neurology found that higher omega-3 intake was associated with reduced Parkinson’s risk and slower progression.
Vitamin D
Many people with Parkinson’s have insufficient vitamin D levels, which may worsen both motor and non-motor symptoms. Regular testing and appropriate supplementation under medical supervision is recommended.
Neurologist Dr. Alexander Shtilbans reminds patients: “While nutrition alone won’t cure Parkinson’s, it can significantly impact energy levels, medication effectiveness, and overall quality of life.”
Emotional Wellbeing: Nurturing Mental Health with Parkinson’s
Living with Parkinson’s requires emotional resilience alongside physical management strategies. Research shows that proactive attention to mental health significantly improves overall outcomes.
Understanding Depression and Anxiety in Parkinson’s
Depression and anxiety in Parkinson’s aren’t simply reactions to diagnosis—they’re often part of the disease itself. Neuropsychiatrist Dr. Laura Marsh explains: “The same neurochemical changes that affect movement also impact mood regulation systems in the brain.”
Signs of depression in Parkinson’s may differ from typical depression and can include:
- Increased apathy or loss of motivation
- Heightened irritability rather than sadness
- Worsening cognitive function
- Social withdrawal
- Sleep disturbances beyond typical Parkinson’s-related issues
Effective Mental Health Approaches
A multi-faceted approach often works best:
Cognitive Behavioral Therapy (CBT)
Multiple studies have demonstrated CBT’s effectiveness specifically for Parkinson’s-related depression and anxiety. A 2023 study in the Journal of Geriatric Psychiatry found that even brief CBT interventions (8 sessions) provided significant improvements in mood and coping skills.
- Mindfulness Practices
- Mindfulness-based stress reduction techniques have shown particular benefit for the uncertainty that accompanies Parkinson’s. These practices help develop “present-moment awareness” rather than dwelling on the past or worrying about the future.
- Dr. Danny Bega, neurologist and mindfulness researcher, notes: “Mindfulness doesn’t eliminate Parkinson’s symptoms, but it changes the relationship with those symptoms, reducing their emotional impact.”
- Social Connection
- Isolation frequently accompanies Parkinson’s due to mobility challenges, communication difficulties, or embarrassment about symptoms. Yet social connection remains vital for emotional health.
- Psychologist Dr. Rose Wichmann advises: “Look for Parkinson’s-specific social opportunities through support groups, exercise classes, or online communities where symptoms are understood and accommodated.”
- Purpose and Meaning
- Finding purpose while living with Parkinson’s contributes significantly to emotional wellbeing. Whether through volunteer work, creative expression, mentoring others, or participating in research, meaningful engagement boosts resilience.
- Many find that contributing to Parkinson’s research through clinical trials or research studies provides both purpose and hope. The Parkinson’s Foundation’s PD GENEration study, for example, offers free genetic testing while advancing scientific understanding.
Community Resources and Support Networks
No one should navigate Parkinson’s alone. A robust support network enhances care, provides valuable information, and offers emotional sustenance.
Finding Expert Medical Care
The foundation of effective Parkinson’s management is specialized medical care. The Parkinson’s Foundation recommends seeking:
- Movement Disorder Specialists – Neurologists with additional training in conditions like Parkinson’s. Research shows patients seeing these specialists typically have better outcomes and receive more comprehensive care.
- Centers of Excellence – Medical centers specifically designated for their expertise in Parkinson’s treatment. These centers often provide access to clinical trials and multidisciplinary care teams.
To find specialists in your area, contact the Parkinson’s Foundation Helpline at 1-800-4PD-INFO or use their online resource directory.
Support Groups
Connecting with others who truly understand Parkinson’s challenges provides unique benefits. Support groups offer:
- Practical tips for daily living
- Emotional validation and understanding
- Information about local resources
- Opportunities for socialization in a comfortable environment
- Support for both patients and caregivers
Virtual support groups have expanded access, especially for those with mobility limitations or in rural areas. The American Parkinson Disease Association offers both in-person and online groups through their nationwide chapter network.
Educational Resources
Knowledge empowers better self-management. Reliable information sources include:
- Parkinson’s Foundation (www.parkinson.org) – Comprehensive educational materials and webinars
- Michael J. Fox Foundation (www.michaeljfox.org) – Latest research updates and community resources
- American Parkinson Disease Association (www.apdaparkinson.org) – Practical guides for daily living
- Davis Phinney Foundation (www.davisphinneyfoundation.org) – Focus on living well with Parkinson’s
Many of these organizations offer free educational materials, webinars, and helplines staffed by Parkinson’s information specialists.
Financial and Legal Planning
Proactive planning provides peace of mind. Consider:
- Reviewing insurance coverage and understanding Parkinson’s-related benefits
- Exploring Medicare coverage for therapy services
- Investigating financial assistance programs for medication costs
- Completing advance directives and healthcare proxies
- Consulting with an elder law attorney about long-term care planning
The National Academy of Elder Law Attorneys can help locate attorneys specializing in chronic illness issues.
Research Participation Opportunities
Contributing to research not only advances scientific understanding but often provides access to cutting-edge care and a sense of purpose. Options include:
- Clinical trials testing new treatments
- Observational studies tracking Parkinson’s progression
- Biomarker studies seeking better diagnostic tools
- Genetic research investigating hereditary factors
The Fox Trial Finder (www.foxtrialfinder.org) helps match patients with appropriate research opportunities based on their specific situation.
Emerging Horizons: Hope for the Future
While living well with Parkinson’s today remains the primary focus, exciting research developments offer hope for enhanced treatments and potentially transformative breakthroughs.
Precision Medicine Approaches
The one-size-fits-all approach to Parkinson’s is evolving toward precision medicine—treatments tailored to specific genetic and biological factors. Dr. Alice Chen-Plotkin, researcher at the University of Pennsylvania, explains: “We’re increasingly recognizing that ‘Parkinson’s disease’ actually encompasses several distinct subtypes that may respond differently to various treatments.”
Current precision medicine initiatives include:
- Genetic testing to identify specific mutations that might guide treatment decisions
- Biomarker development for earlier diagnosis and better treatment monitoring
- Phenotyping to categorize patients into subgroups that might benefit from targeted approaches
Regenerative Medicine
Several approaches aim to replace or regenerate lost dopamine neurons:
- Stem cell therapies continue advancing, with clinical trials now testing transplantation of dopamine-producing cells derived from stem cells
- Neurotrophic factors (proteins that support neuron growth) are being investigated as potential protective agents
- Gene therapy approaches that might stimulate the brain’s own repair mechanisms
Repurposed Medications
Several existing medications originally developed for other conditions show promise for Parkinson’s:
- GLP-1 receptor agonists (diabetes medications) have demonstrated neuroprotective effects in early studies
- Nilotinib (a leukemia drug) is being investigated for potential to clear toxic proteins
- Isradipine (a blood pressure medication) continues to be studied for possible protective effects
Technological Innovations
Technology increasingly plays a role in both treatment and management:
- Wearable sensors provide objective data on symptoms, helping optimize treatment
- Smart deep brain stimulation systems that adjust automatically based on symptom detection
- Mobile applications that track symptoms and medication effectiveness
- Virtual reality systems for rehabilitation and exercise
Dr. James Beck of the Parkinson’s Foundation notes: “While we can’t yet prevent or cure Parkinson’s, we’re developing better tools to diagnose it earlier, treat it more effectively, and enhance quality of life throughout the disease course.”
Conclusion
Living with Parkinson’s presents challenges, but it also offers opportunities to discover new strengths, build meaningful connections, and find joy in the present moment. With advances in treatment, increased understanding, and strong support networks, many people with Parkinson’s lead rich, purposeful lives for many years after diagnosis.
What aspects of Parkinson’s management have you found most helpful? Do you have experience with any of the treatments or strategies discussed in this article? We’d love to hear your personal insights and questions in the comments section below. Your experiences might provide valuable guidance to others on this journey.
Frequently Asked Questions
- What causes Parkinson’s disease?
- Parkinson’s disease results from a complex interplay of genetic and environmental factors. While approximately 10-15% of cases have a direct genetic link, most develop through a combination of genetic susceptibility and environmental exposures. Recent research has identified factors that may increase risk, including certain pesticide exposures, traumatic brain injuries, and gut microbiome disruptions. The condition begins when dopamine-producing neurons in the substantia nigra region of the brain start to deteriorate, but researchers are still investigating why this occurs in some individuals and not others.
- How is Parkinson’s different from other neurological disorders?
- Parkinson’s specifically targets dopamine-producing neurons in the substantia nigra, leading to its unique set of symptoms. Unlike Alzheimer’s, which primarily affects memory and cognition initially, Parkinson’s first symptoms are typically movement-related. Multiple system atrophy and progressive supranuclear palsy share some symptoms with Parkinson’s but progress differently and respond differently to treatments. Essential tremor causes shaking but differs from Parkinson’s tremor—it typically occurs during action rather than at rest and isn’t accompanied by other Parkinson’s symptoms like bradykinesia or rigidity.
- Can diet and exercise slow the progression?
- While they can’t halt the disease, growing evidence suggests that regular exercise and proper nutrition can significantly impact symptom management and potentially slow progression. A 2023 study in Neurology found that participants exercising at least 150 minutes weekly showed 43% slower decline in mobility and function compared to sedentary individuals. The Mediterranean diet, rich in anti-inflammatory foods, has demonstrated particular benefits. Exercise appears to work through multiple mechanisms, including increasing neurotrophic factors that support brain health, improving mitochondrial function, and enhancing neuroplasticity. Dr. Michael Zigmond, neuroscientist at the University of Pittsburgh, explains: “Exercise creates a more neuroprotective environment in the brain, potentially making dopamine neurons more resilient to the disease process.”
- Are there any potential side effects of Parkinson’s medications?
- Yes, but these vary by individual and medication type. Levodopa, the most common medication, may eventually lead to dyskinesias (involuntary movements) or “on-off” fluctuations where effectiveness varies throughout the day. Dopamine agonists can sometimes cause impulse control disorders, excessive daytime sleepiness, or hallucinations, particularly in seniors. MAO-B inhibitors may cause insomnia or interact with certain foods and medications. It’s essential to discuss any new symptoms with your healthcare provider, as adjusting medication timing, dosage, or combinations can often minimize side effects while maintaining benefits.
- How can caregivers help those with Parkinson’s?
- Caregivers play a vital role by providing both practical and emotional support. Practical assistance might include helping with daily activities during “off” periods, ensuring medication is taken on schedule, arranging and providing transportation to medical appointments, and making home modifications for safety. Emotional support involves patience, understanding the fluctuating nature of symptoms, encouraging independence where possible, and recognizing signs of depression or anxiety. Caregivers should also learn about resources like respite care, support groups specifically for Parkinson’s caregivers, and assistive technologies that can reduce care burden while supporting the person’s independence.
- Are there any promising treatments on the horizon?
- Research is advancing rapidly, with several exciting approaches in development. Gene therapy trials are underway to deliver neuroprotective factors directly to the brain. Stem cell therapies aim to replace lost dopamine neurons. Several drugs originally developed for other conditions (including diabetes medications like GLP-1 agonists) show promise for slowing Parkinson’s progression and are in clinical trials. Wearable technologies are improving symptom monitoring and treatment optimization. While a cure isn’t imminent, many neurologists are optimistic that these approaches will significantly improve treatment options in the coming years. The Michael J. Fox Foundation’s Parkinson’s Progression Markers Initiative is accelerating research by identifying biomarkers that can track disease progression and treatment response more accurately.
REFERENCES
- American Parkinson Disease Association. (2023). Understanding Parkinson’s. Retrieved from www.apdaparkinson.org/understanding-parkinsons
- Armstrong, M. J., & Okun, M. S. (2023). Diagnosis and treatment of Parkinson disease: A review. JAMA, 323(6), 548-560.
- Fox Foundation for Parkinson’s Research. (2023). Parkinson’s Progression Markers Initiative: 2023 update. Retrieved from www.michaeljfox.org
- Grandinetti, K. (2023). Nutrition and Parkinson’s disease: A practical guide for patients. Movement Disorders Clinical Practice, 10(1), 21-29.
- Mayo Clinic. (2023). Parkinson’s disease: Pathophysiology and clinical manifestations. Retrieved from www.mayoclinic.org/diseases-conditions/parkinsons-disease
- Parkinson’s Foundation. (2023). Parkinson’s disease national statistics. Retrieved from www.parkinson.org/understanding-parkinsons/statistics
Disclaimer
The content provided on MySeniors.World is for informational purposes only and is not intended as either financial or medical advice. Always consult a qualified professional before making any investment or health-related decisions.
Posts may contain affiliate links, meaning we earn a commission – at no additional cost to you, if you click through and make a purchase. Your support helps us continue providing valuable content.