Varicose Veins in Seniors: Causes, Care, and Smart Solutions

Last Updated on July 2, 2025 by Rose Ann
Are you noticing those twisted, rope-like veins on your legs becoming more prominent? You’re not alone. Varicose veins affect millions of adults, particularly those in their retirement years, but here’s the encouraging news: today’s treatment options are more effective and less invasive than ever before.
This comprehensive guide explores everything you need to know about managing varicose veins as a mature adult. We’ll uncover the surprising causes beyond just genetics and aging—including how hormonal changes during menopause and lifestyle factors play crucial roles. You’ll discover why that heavy, aching feeling in your legs after standing isn’t something you have to “just live with.”
From simple lifestyle adjustments that can provide immediate relief to cutting-edge medical treatments that require minimal downtime, we cover all your options. You’ll learn about the remarkable effectiveness of graduated compression stockings, natural remedies that really work, and when it’s time to consider professional intervention.
We’ll also address common concerns: Are these treatments safe for mature adults? What can you expect during recovery? How do you choose between sclerotherapy, laser therapy, and newer techniques?
Most importantly, you’ll discover that varicose veins don’t have to limit your active lifestyle. With the right approach, whether that’s prevention strategies, non-invasive treatments, or medical procedures, you can maintain healthy circulation and comfortable legs throughout your retirement years.
Ready to take the first step toward healthier veins and more comfortable days? Let’s explore your options together.
Recognizing Varicose Veins
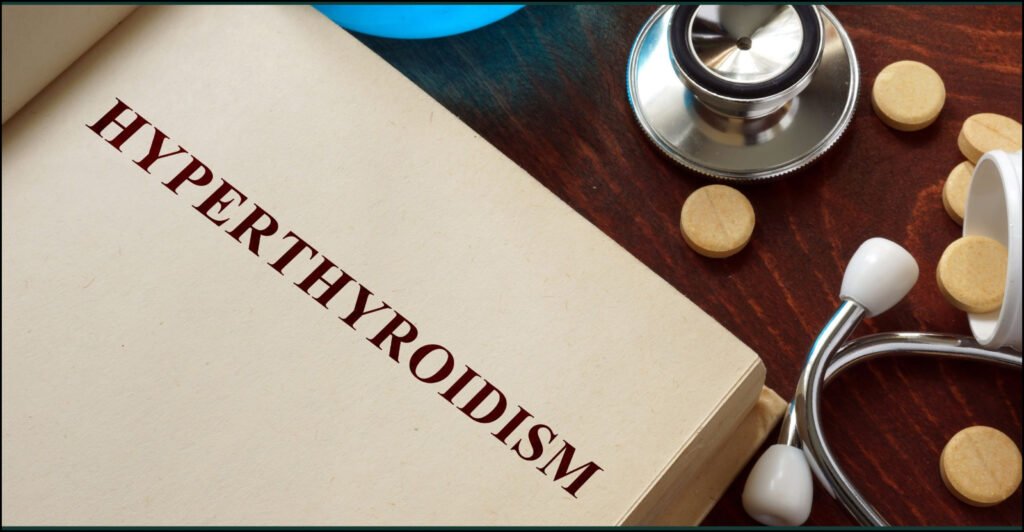
Varicose veins appear as enlarged, dark blue or purple veins, typically on the legs, giving the impression of bulging or rope-like cords beneath the skin. You might notice them accompanied by a heavy or aching sensation in your legs, especially after standing for extended periods.
It’s essential to recognize these signs early to manage the condition effectively and prevent further complications. Varicose veins develop when atypical or damaged valves in the veins allow blood to flow in the wrong direction or to pool.
Normally, these one-way valves are crucial in maintaining the flow of blood toward the heart, working against gravity. When these valves malfunction, blood can collect or pool in the veins, causing increased pressure and distension. This results in the characteristic appearance of varicose veins.
Prefer to listen rather than read?
The affected veins may appear blue or purple due to the deoxygenated blood they contain. Risk factors include family history of venous disease; female sex; older age; chronically increased intra-abdominal pressure due to obesity, pregnancy, chronic constipation, or a tumor; and prolonged standing.
The likelihood of developing varicose veins increases significantly as we mature. This can be attributed to various factors associated with the natural aging process. Over time, the veins undergo wear and tear, causing them to become less resilient and more susceptible to damage.
Additionally, circulation tends to decline with age, potentially worsening the development of varicose veins. Reduced blood flow and compromised venous return can lead to blood pooling in the veins, causing pressure and stretching that results in the characteristic bulging appearance.
Understanding the Aging Connection
Mature adults may also experience hormonal changes that can significantly impact vein health. During menopause, for example, hormonal fluctuations can affect the integrity of the veins and their ability to maintain proper blood flow.
Additionally, some muscle tone changes during the aging process can impact vein health. When supporting muscles aren’t as strong as they once were, this can result in elevated pressure on the veins and contribute to varicose vein development.
It’s important for mature adults to be aware of these age-related factors and their potential influence on varicose veins, while understanding that effective management and treatment options are readily available.
Causes of Varicose Veins in Seniors
Several factors contribute to the development of varicose veins in seniors. Understanding these causes can help in both prevention and treatment decisions.
Age and Genetics
As individuals mature, their blood vessels undergo natural changes that impact their elasticity, leading to some loss of natural strength and resilience. This age-related evolution in vein health can contribute to the development of varicose veins.
Furthermore, some individuals have a genetic predisposition to weakened vein valves, which increases their likelihood of developing this condition. The combination of natural aging processes and genetic factors creates an environment where varicose veins are more likely to occur.
Prolonged Sitting or Standing
Adults who spend extended periods sitting or standing—whether due to work requirements, limited mobility, or lifestyle factors—are at higher risk of developing varicose veins. Extended periods without regular movement can lead to poor blood circulation in the legs.
When circulation becomes compromised, blood may accumulate and pool in the veins, exerting increased pressure on their walls. Over time, this elevated pressure can weaken the vein walls and contribute to varicose vein formation.

Therefore, it’s essential to incorporate physical activity and regular movement into daily routines to promote healthy blood flow and reduce risk. A diet packed with circulation-boosting foods like vegetables, fruits, lean meats, and fish keeps veins healthy. Combined with regular exercise, a healthy diet takes the stress off your veins by keeping your weight at an ideal level.
Engaging in regular, appropriate exercise plays a crucial role in maintaining healthy blood circulation and preventing varicose veins. Through exercise, the leg muscles responsible for pumping blood back to the heart become stronger and more efficient. This improved muscle strength enhances overall blood flow in the lower extremities, reducing the likelihood of blood pooling in the veins.
Hormonal Changes
Hormonal fluctuations, particularly during menopause, can have a significant impact on vein health in mature adults. During this stage, the body experiences changes in hormone levels, specifically a decrease in estrogen production.
Estrogen plays a vital role in maintaining the elasticity and strength of vein walls and valves. As estrogen levels decline, the vein walls and valves may weaken, becoming more susceptible to dilation and varicose vein formation.
The hormonal shifts during menopause create conditions where varicose veins are more likely to develop. Understanding the influence of hormones on vein health emphasizes the importance of comprehensive care and management for adults experiencing menopause-related varicose veins.
Symptoms and Complications
Identifying the symptoms of varicose veins is crucial for early detection and prompt treatment. While each individual may experience different symptoms, the following are commonly associated with this condition:
Visible Enlarged Veins
One of the primary indicators of varicose veins is the visible presence of twisted and bulging veins on the skin’s surface. These veins, often found in the legs, take on a distinct bluish or purplish hue. The twisted nature of varicose veins results from weakened vein walls and valves, causing blood to pool and the veins to enlarge.
This enlargement creates a noticeable protrusion that can be both seen and felt. The bluish or purplish coloration occurs due to the deoxygenated blood within the veins. Recognizing these characteristic visual cues helps individuals identify varicose veins and seek appropriate medical attention and treatment.
Leg Pain and Discomfort
Adults who experience varicose veins often endure a range of uncomfortable symptoms in the affected leg. Symptoms of varicose veins include a heavy, achy feeling and an itching or burning sensation; these symptoms worsen with prolonged standing.
The severity of these sensations may vary, ranging from mild discomfort to more intense pain. Extended periods of standing or sitting can worsen these symptoms by impeding proper blood flow, leading to increased pressure in the affected veins and intensified aching and throbbing.
The heaviness in the leg may feel burdensome and can impact mobility, making daily activities more challenging. To alleviate these symptoms, adults are encouraged to engage in regular leg movement, elevate their legs when resting, and consider wearing compression stockings.
Swelling and Edema
Varicose veins often result in swelling in the legs and ankles, a condition known as edema. The pooling of blood in the affected veins hinders efficient fluid drainage, leading to fluid retention in the surrounding tissues.
This accumulation of fluid causes the legs and ankles to become swollen, which can be uncomfortable and may restrict mobility. The swelling may range from mild to more pronounced, depending on the severity of the varicose veins. The increased pressure and fluid buildup can cause a sensation of tightness and heaviness in the affected areas.
Adults with edema may experience mobility challenges due to discomfort. Lifestyle changes like appropriate exercise, leg elevation, and compression therapy can help ease swelling and improve comfort. Seeking medical advice is crucial for effective management.
Skin Changes and Ulcers
More advanced cases of varicose veins can lead to notable skin changes that include dryness, itchiness, and discoloration. The affected skin may become dry and prone to irritation, leading to persistent itchiness. Additionally, compromised blood flow and nutrient supply to the skin can cause discoloration, appearing darker or mottled.
Moreover, the skin’s condition due to compromised circulation can make it more vulnerable to developing ulcers in severe cases. These ulcers can be painful and slow to heal, posing additional challenges for individuals dealing with advanced varicose veins.
It’s crucial for adults with significant varicose veins to seek medical attention and explore appropriate treatment options to prevent and manage these skin changes effectively, ensuring improved comfort and promoting healing.
Prevention and Lifestyle Changes
While it may not be possible to prevent varicose veins entirely, mature adults can adopt certain lifestyle changes to lower their risk and effectively manage associated symptoms.
Regular exercise, maintaining a healthy weight, avoiding prolonged sitting or standing, and elevating legs all benefit blood circulation. Exercise strengthens the muscles that help pump blood back to the heart, while maintaining an appropriate weight reduces strain on veins and prevents blood pooling.
Periodic leg elevation aids in reducing swelling and enhancing venous return. By incorporating these lifestyle modifications, adults can significantly minimize the occurrence of varicose veins and enjoy improved vascular health.
Medical Treatments for Varicose Veins
Management options include lifestyle modifications, compression therapy, local ablative therapies, surgical interventions, and endovenous ablative therapies. These medical treatments offer viable solutions for adults with more significant varicose veins.
It’s important for individuals to consult with a healthcare professional to determine the most suitable treatment option based on their specific condition and overall health. By exploring these procedures, mature adults can effectively address their varicose veins, alleviate symptoms, and improve their overall vascular health and quality of life.
Sclerotherapy
Sclerotherapy is a widely used medical procedure for treating varicose veins. It involves injecting a specialized solution directly into the affected veins. The solution irritates the vein walls, causing them to collapse and stick together.

Over time, the closed-off veins are reabsorbed by the body, redirecting blood flow to healthier veins. Sclerotherapy is typically performed as an outpatient procedure, and multiple sessions may be required for optimal results.
Laser Therapy
Endovenous laser ablation (EVLA) is a cutting-edge treatment for varicose veins that utilizes laser energy to seal and collapse the affected veins. During the procedure, a thin laser fiber is inserted into the vein under ultrasound guidance and laser energy is delivered to heat and seal the vein.
Similar to sclerotherapy, the body eventually absorbs the closed vein, rerouting blood to healthier pathways. Laser therapy is performed under local anesthesia, and patients can typically resume normal activities shortly after the procedure.
Endovenous Ablation
Endovenous ablation is a minimally invasive procedure used to treat varicose veins. Various treatment options, including minimally invasive techniques such as endogenous laser ablation, sclerotherapy, and radiofrequency ablation, are available for varicose veins across the globe. These treatment options are primarily preferred due to their benefits such as reduced pain, shorter recovery times.
This targeted energy causes the vein to collapse and seal shut. The body gradually absorbs the closed vein, redirecting blood flow to healthier veins. Endovenous ablation is performed on an outpatient basis and usually requires only local anesthesia. Recovery time is minimal, allowing patients to resume daily activities soon after the procedure.
Advanced Treatment Options
Unlike a few decades ago, there are now a number of minimally invasive ways to treat varicose veins. Doctors can shut down problem veins with various injections or catheter procedures. A treatment now under study would “zap” away varicose veins with focused ultrasound waves.
Newer treatments include cyanoacrylate glue, mechanochemical ablation, and endovenous steam ablation, offering patients even more options for effective treatment.
Non-Surgical Options for Seniors
Not all treatments require surgical intervention. There are effective non-surgical options available, particularly compression therapy.
Natural Remedies for Varicose Veins
Elevating the legs above the level of the heart, particularly during periods of rest or sleep, is an effective method for reducing blood pooling and alleviating swelling commonly associated with varicose veins.

By raising the legs, gravitational force is counteracted, allowing blood to flow more easily from the lower extremities back toward the heart. This positioning helps improve overall blood circulation, preventing the accumulation of blood in the affected veins.
As a result, the swelling and discomfort caused by varicose veins are diminished, providing relief and promoting better vein health. Regular leg elevation, along with other lifestyle modifications, can be a valuable self-care practice for managing varicose veins and enhancing overall well-being.
Dietary Recommendations
Maintaining a healthy diet plays a crucial role in supporting vein health and minimizing the risk of varicose veins, especially for mature adults. It’s recommended to prioritize a balanced diet that includes an abundance of fruits, vegetables, whole grains, and lean proteins.
These nutrient-rich foods provide essential vitamins, minerals, and fiber that contribute to overall vein health. In particular, incorporating foods high in antioxidants and flavonoids, such as berries and leafy greens, can help strengthen blood vessels and improve their elasticity.
Antioxidants combat oxidative stress, which can damage veins, while flavonoids promote healthy blood circulation and reduce inflammation. By adopting a diet focused on these elements, mature adults can nourish their veins, reduce the likelihood of varicose veins, and support optimal vascular function.
Compression Stockings and Clothing
Compression stockings may not eliminate varicose veins, but they may reduce associated pain and swelling. Compression socks can reduce swelling and leg fatigue caused by the condition.
Compression stockings work by applying external pressure on the veins. This external pressure is meant to ease blood flow through the veins by creating a more favorable pressure gradient across the vein.

Adults can derive maximum advantage by selecting compression stockings that provide the appropriate level of compression as recommended by healthcare professionals. Furthermore, choosing loose-fitting clothing that doesn’t constrict the waist or legs allows unrestricted circulation.
Avoiding tight waistbands or belts can prevent impeded blood flow and provide additional support to vein health. Compression socks and stockings might not always prevent varicose veins from developing. However, they can function as a great supportive mechanism for a healthy blood flow and keep bothersome symptoms at bay, especially when worn on a long-term basis.
Cold and Warm Compresses
Cold and warm compresses are simple yet effective methods for obtaining temporary relief from the pain and swelling associated with varicose veins. When experiencing discomfort, applying a cold compress, such as a cold pack or a cloth soaked in cold water, can help reduce inflammation and numb the area, providing immediate soothing relief.
Conversely, warm compresses, such as a warm towel or a heating pad set to a gentle temperature, can enhance blood circulation and relax the affected muscles, relieving pain and reducing swelling. Alternating between cold and warm compresses can also be beneficial, as it promotes blood flow while simultaneously providing a calming effect.
However, it’s important to note that compresses offer temporary relief and do not treat the underlying cause of varicose veins. For long-term management and comprehensive treatment, consultation with a healthcare professional is recommended.
Conclusion
Varicose veins can be a common concern for mature adults, causing discomfort and potentially leading to complications if left unaddressed. However, with the right approach and awareness, adults can manage their varicose veins effectively and maintain an active, comfortable lifestyle.
From simple lifestyle changes and natural remedies to advanced medical treatments, today’s options are more effective and less invasive than ever before. Whether you’re dealing with early-stage symptoms or more advanced varicose veins, there are solutions available that can significantly improve your comfort and quality of life.
The key is understanding your options and working with healthcare professionals to develop a personalized approach that fits your lifestyle and health needs. Remember, you don’t have to simply “live with” the discomfort of varicose veins, effective help is available.
Are you currently managing varicose veins, or do you have questions about the treatment options we’ve discussed? We’d love to hear about your experiences and any strategies that have worked well for you. Please share your thoughts in the comments below, your insights might help fellow readers on their journey to healthier, more comfortable legs.
Disclaimer
The content provided on MySeniors.World is for informational purposes only and is not intended as either financial or medical advice. Always consult a qualified professional before making any investment or health-related decisions.
Posts may contain affiliate links, meaning we earn a commission – at no additional cost to you, if you click through and make a purchase. Your support helps us continue providing valuable content.
Frequently Asked Questions About Varicose Veins
- At what age do varicose veins typically become a concern?
- While varicose veins can develop at any age, they become more common as we mature, particularly after age 50. Risk increases with age due to natural changes in vein elasticity and valve function, but they’re not inevitable—many people never develop them regardless of age.
- Are compression stockings really effective, and how long should I wear them?
- Yes, compression stockings are highly effective for managing varicose vein symptoms. Research shows they can significantly reduce pain, swelling, and leg fatigue. Most healthcare providers recommend wearing them during the day when you’re active, removing them at night. The key is consistent daily use for maximum benefit.
- Can varicose veins be dangerous if left untreated?
- While most varicose veins are primarily a cosmetic concern, some can lead to complications including skin ulcers, blood clots, or chronic swelling. It’s important to have them evaluated by a healthcare professional, especially if you experience significant pain, skin changes, or swelling.
- Will exercise make my varicose veins worse?
- Actually, appropriate exercise often helps varicose veins by strengthening the muscles that assist blood flow back to your heart. Low-impact activities like walking, swimming, and cycling are particularly beneficial. High-impact activities might temporarily increase symptoms, but regular exercise generally improves overall vein health.
- How do I know if I need medical treatment versus lifestyle changes?
- Consider medical evaluation if you experience significant pain, swelling that doesn’t improve with elevation, skin changes around the veins, or if symptoms interfere with your daily activities. A vascular specialist can assess severity and recommend the most appropriate treatment approach.
- Are newer varicose vein treatments safe for people in their 70s and 80s?
- Many modern varicose vein treatments are specifically designed to be safer for mature adults. Procedures like sclerotherapy and laser treatments are minimally invasive with lower risk profiles than traditional surgery. Your doctor will evaluate your overall health to determine the safest, most effective options for your situation.
- Can diet really make a difference in varicose vein management?
- Absolutely. A diet rich in fiber helps prevent constipation (which can worsen varicose veins), while foods high in flavonoids and antioxidants support vein health. Maintaining a healthy weight through proper nutrition also reduces pressure on your veins. Stay hydrated to support good circulation.
- What’s the difference between spider veins and varicose veins?
- Spider veins are smaller, closer to the skin surface, and appear as thin red or blue lines. Varicose veins are larger, deeper, and often bulge above the skin surface. While spider veins are primarily cosmetic, varicose veins are more likely to cause symptoms and complications.
References
- Medical News Today. (2024, December 17). Varicose veins: Causes, symptoms, treatment. Retrieved from https://www.medicalnewstoday.com/articles/240129
- American Academy of Family Physicians. (2019, June 1). Varicose Veins: Diagnosis and Treatment. Retrieved from https://www.aafp.org/pubs/afp/issues/2019/0601/p682.html
- Encino Vascular. (2024, October 25). The Top Vein Treatments in 2024. Retrieved from https://encinovascular.com/blog/the-top-vein-treatments-in-2024/
- Harvard Health Publishing. (2023, June 1). Advances in varicose vein treatment. Retrieved from https://www.health.harvard.edu/diseases-and-conditions/advances-in-varicose-vein-treatment
- Yale Medicine. (2024, June 17). Blood Clots, Varicose Veins, and Sore Legs: Can Compression Socks Help? Retrieved from https://www.yalemedicine.org/news/blood-clots-varicose-veins-sore-legs-compression-socks-help
- Medical News Today. (2023, July 28). Compression stockings for varicose veins: Benefits and risks. Retrieved from https://www.medicalnewstoday.com/articles/321662
- Center for Vein. (2023, August 10). Why Seniors Should Seek Varicose Veins Treatment. Retrieved from https://www.centerforvein.com/blog/why-seniors-should-seek-varicose-veins-treatment
- American Heart Association. Circulation Journal. Varicose Veins Management Guidelines. Retrieved from https://www.ahajournals.org/doi/10.1161/circulationaha.113.008331