Yes, Seniors Are Having Sex: Why Doctors Still Don’t Ask

Last Updated on February 16, 2026 by George
Picture your 72-year-old mom finally working up the nerve to mention that sex has started to hurt. The doctor quickly pivots to her blood pressure meds, as if she didn’t say anything important. Then your 68-year-old dad started dating again. He sees his cardiologist and does not get asked about his new sex life. This is an important detail as it could affect his heart condition.
Moments like these happen all the time. They point to a bigger issue in healthcare: the quiet assumption that older adults stop having sex or shouldn’t be talking about it. The problem is that the assumption doesn’t match reality. Research keeps showing that many seniors are still sexually active. Including studies that put the number at more than half of people aged 65 to 80.
When doctors skip these conversations, it doesn’t just feel awkward or dismissive. It creates a blind spot. Pain, dryness, infections, medication side effects, erectile issues, and even heart-related risks can be addressed. This happens when no one is asking the basic questions. When patients sense discomfort or judgment, they’re less likely to bring it up again. This can turn into a real health concern into an ongoing silence.

Key Takeaways
- Many doctors still assume older adults aren’t sexually active, so real issues like pain, dryness, erectile changes, STI risk, and medication side effects get ignored.
- Awkwardness and rushed appointments keep both patients and providers silent, which turns treatable sexual health problems into long-term stress and discomfort.
- Sexual health is part of whole-body health in later life, and speaking up helps protect quality of life while pushing healthcare to treat seniors as complete people.
Understanding the Doctor-Patient Disconnect
A lot of healthcare settings still treat senior sexuality as an awkward subject. This prevents doctors from bringing it up. That silence doesn’t happen by accident. It usually comes from age-based assumptions. In fact, many clinicians were never really taught how to talk about sexual health with older adults.
The impact of ageist assumptions in clinical settings
Many providers carry an unspoken belief that sexual desire and sex itself fade out after a certain age. Even when no one says it out loud, it shows up in the way visits get handled. The conversion stays locked on other medical problems like blood pressure and diabetes. Doctors tend to skip anything related to sex.
The problem is that this mindset that older couples are not sexually active creates a real gap in senior care. Doctors miss chances to ask about medical issues related to sex, like dryness or erectile changes. There are even important topics like STI risks and medication side effects that are not being brought up. The emotional side is also ignored. That part could be a big part of a senior’s connection and quality of life.
Generational discomfort and the communication gap
Awkwardness cuts both ways. Many older patients were raised in a culture where sex wasn’t discussed openly, especially with authority figures. They may worry they’ll be judged, brushed off, or told it’s “normal at your age,” so they keep quiet even when something is wrong.
Doctors can feel uncomfortable too. Some don’t know how to ask without sounding intrusive. Others worry they’ll embarrass the patient or open a conversation they don’t have time to handle properly. So both sides hesitate, and the easiest thing to do becomes saying nothing. That’s how treatable issues turn into years of discomfort, stress, and guessing.
Inadequate medical training and time constraints
Most medical training spends a lot more time on sexual health in younger people than it does on the realities of aging. Clinicians may learn plenty about reproduction, contraception, and pregnancy, but get very little guidance on menopause-related pain, erectile changes linked to vascular health, the impact of common meds, or how chronic conditions affect sexual function and safety.
Then there’s time. Many appointments are rushed, and providers feel pressure to stick to a tight checklist. When that happens, sexual health can get treated like an optional topic instead of a basic part of overall health. The result is a routine, predictable silence, even when the patient is sitting right there hoping someone will ask.

The Reality: Seniors Are Still Having Sex
The idea that intimacy has an expiration date is one of those aging myths that just won’t quit. Real life doesn’t match it. For many people, the desire for closeness, touch, and sex stays very real through the seventies, eighties, and beyond.
Redefining Intimacy in the Golden Years
Movies and TV love to act like romance belongs to the young. A lot of older adults will tell you the opposite. With age, intimacy often feels less performative and more personal. There’s usually less pressure to prove anything. You have more room to focus on comfort, trust, and what actually feels good.
Life changes can reshape how intimacy looks, too. Pregnancy worries drop off the table. Work and child-raising pressures aren’t as loud. Some people find they finally have time and privacy again. Others are rebuilding after a divorce or the loss of a partner. They’re learning how to date with a clear sense of what they want. The details change, but the basic need for connection doesn’t just disappear as you grow older.
What the Statistics Actually Reveal
The numbers back this up. Research has repeatedly found that a large share of adults in the 65–80 range are still sexually active, and many say intimacy matters to their happiness and quality of life. In other words, this isn’t rare or unusual. It’s normal, it’s common, and it deserves to be treated that way in healthcare conversations and in everyday life.
Navigating New Relationships and Modern Dating
Dating later in life looks different than it did at 25, but it’s not some strange exception. Online dating, social groups, and senior communities have made it easier for people to meet. Many older adults also come into dating with fewer games and more clarity. They know what they’re willing to tolerate and what they’re not.
This shift matters for health reasons too. New relationships can mean new sexual health questions, even if someone hasn’t had to think about that side of things in years. Staying informed isn’t about fear. It’s about being practical and taking yourself seriously.
The Physical and Emotional Benefits of Staying Active
Intimacy isn’t just about sex. It can lower stress, help with sleep, and deepen a sense of safety with a partner. For some couples, it’s one of the few parts of life that still feels like “us” when everything else is changing, especially when health issues or grief are in the picture.
None of this is about trying to look young or chasing an old version of yourself. It’s about letting older age include the full range of human life, including affection, desire, and closeness, if that’s something you want.

The Broader Implications: Why This Matters for Senior Health
Sexual health isn’t some nice-to-have topic you bring up only if there’s extra time. It’s part of your overall health, right alongside sleep, diet, mobility, and mental well-being, especially as your body changes with age.
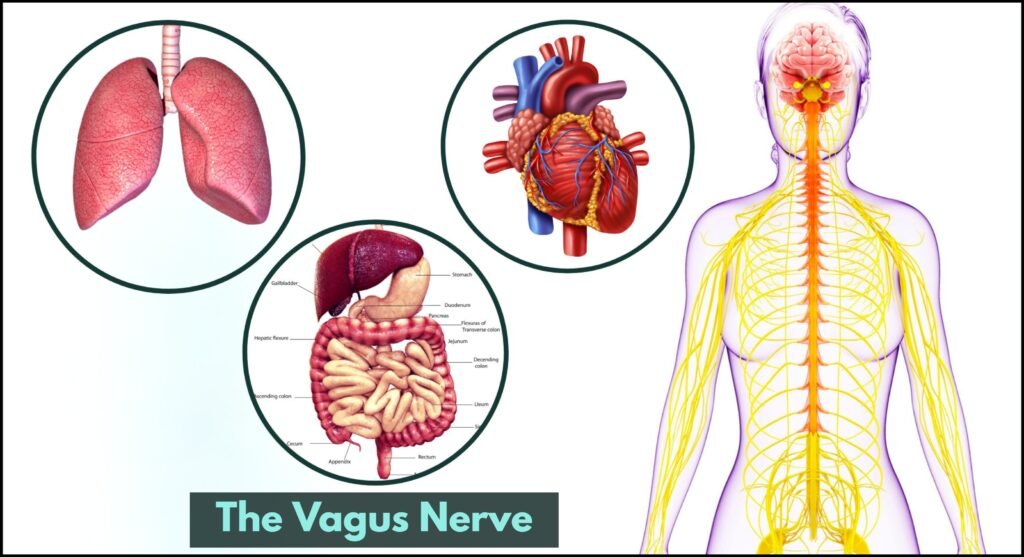
Sexual Wellness as a Barometer for Physical Health
Sexual changes can sometimes be your body’s way of waving a small flag before bigger problems show up. For many men, trouble with erections can point to circulation or heart-related issues. This comes from the reliance on a healthy blood flow for an erection. For many women, pain, dryness, or discomfort during sex can signal medical problems. These issues include vaginal tissue changes after menopause or hormone-related shifts. Both of these are treatable.
The key point is simple: these symptoms aren’t just against in a way you have to accept and live with. They are vital information. Bringing them up can help uncover what’s really going on and steer you toward the right fix.
The Connection Between Intimacy and Mental Clarity
Intimacy isn’t only physical. Feeling close to someone, being touched, and sharing affection can steady you emotionally. There’s also a real body-brain link here. Sex and physical closeness can release chemicals like oxytocin and endorphins that support mood and help the body relax. For people dealing with loneliness, grief, or big life changes in retirement, that sense of connection can matter a lot.
This doesn’t mean sex is a cure for depression or anxiety. It just means emotional closeness and physical intimacy can be a meaningful part of staying grounded and engaged, rather than feeling cut off or isolated.
Challenging Ageism to Improve the Standard of Care
When older patients bring up sexual health, it pushes back against a quiet kind of ageism in medicine. Too often, providers focus only on chronic conditions and ignore the parts of life that make those years worth living. Speaking up helps remind your care team that you’re not just a list of diagnoses. You’re a whole person with real needs and a real relationship life.
It also makes it easier for the next patient. Every time someone treats the topic as normal, it becomes easier for clinicians to do the same.
Quality of Life and the Right to Vitality
Good health isn’t only about avoiding illness. It’s also about enjoying your life, feeling connected, and feeling like yourself. A satisfying intimate life can support that, not because it makes you “young again,” but because it’s one of the ways people feel loved, confident, and alive.
Prioritizing sexual health is basically self-respect. You deserve care that takes it seriously and supports your right to pleasure, closeness, and dignity at any age.
Conclusion
The quiet way sexual health gets skipped in senior checkups is more than awkward. It can block you from getting complete care. Intimacy doesn’t stop being part of health just because you’re older, and it shouldn’t be treated like a side topic that only matters to younger people.
When you name what’s going on and bring it into the open, you’re not asking for special treatment. You’re asking to be treated like a whole person. Sexual health connects to physical comfort, medication side effects, sleep, mood, relationships, and sometimes bigger medical issues that need attention. Talking about it is one practical way to protect your quality of life, not just your lab results.
FAQ
- Why is my doctor hesitant to bring up sexual health during my checkups?
- A lot of doctors simply don’t ask because they assume older patients aren’t having sex, or they worry they’ll embarrass you. Some were never trained to handle sexual health conversations with older adults, so they stick to what they know: chronic conditions and routine screenings. The end result is the same, though. Real concerns get missed even when they’re common and treatable.
- Is it normal to still have a strong desire for intimacy in my 70s or 80s?
- Yes. Wanting touch, closeness, and sex doesn’t come with an age cutoff. The way intimacy looks can change with time, health, and comfort, but the desire for connection is still a normal part of being human.
- Can my regular medications affect my sex life as I get older?
- They can. Many common medications, including some for blood pressure, heart conditions, and depression, can affect libido, arousal, dryness, or erectile function. It’s worth bringing up because there may be options, like adjusting the dose, switching medications, or treating a side effect directly.
- What are the risks of ignoring sexual health concerns in later life?
- A few things can happen. Ongoing pain or dysfunction can create stress in a relationship and chip away at confidence. Some issues can also point to larger health problems, since sexual function is closely tied to hormones, circulation, nerves, and overall wellness. Sexual health is also part of basic prevention, and older adults can still get STIs, especially when they’re dating again.
- How can I start a conversation about sex with a doctor who seems uncomfortable?
- Keep it simple and medical. Try something like: “I’m having a change in my sexual health and I want to talk about it.” If it helps, mention the specific symptom first, like pain, dryness, erectile changes, or low desire. If the response is dismissive, it’s reasonable to ask for a referral to someone who deals with this often, like a gynecologist, urologist, or pelvic health specialist.